Workplace Wellness
by Jennifer Rooke, MD, MPH, FACOEM, FACPM
Employee health costs generally fall into three categories, the cost of workers compensation premiums, the cost of health benefit plans, and the cost of lost productivity due to poor employee health. A recent analysis of the full cost of employee health found that the indirect costs associated with lost productivity from poor employee health had a far greater economic impact on a business than the first two direct costs.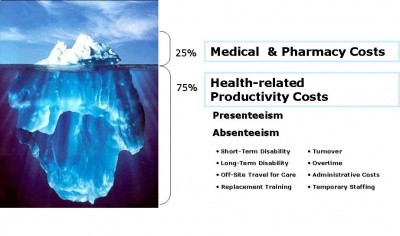
Poor employee health is reflected in measures of absenteeism and presenteeism. The impact of absenteeism is obvious, employees are not at work to complete the tasks that they are paid to perform. Presenteeism is not as obvious and may be a new concept for many people. Presenteeism means that employees are present at work but their productivity is impaired by one or more health conditions or social problems. The resulting poor work performance may cost an employer as much as 4 times the direct costs of doctor’s visits and medications. You can see from the chart below that some health conditions cost employers more than others.
Top 10 Doctor Diagnosed Health Conditions by Annual Medical, Drug, Absenteeism and Presenteeism Costs/1000 Full Time Workers
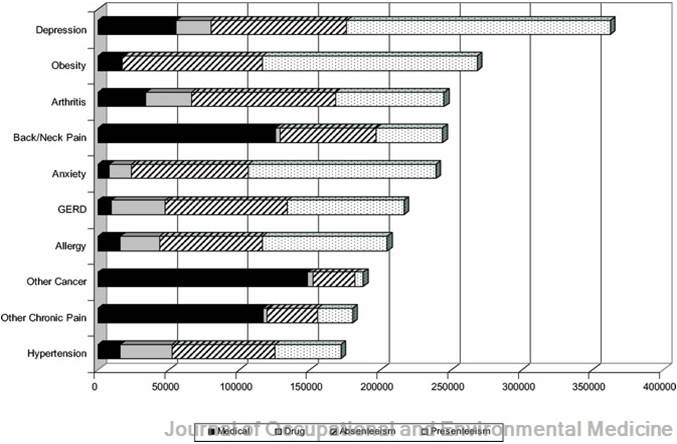
An effective workplace wellness program would target the costliest health problems, improve health and productivity, and produce a return on investment (ROI) for employers. The seven costliest health conditions are:
Depression and anxiety
Chronic pain – arthritis, back, neck and other pain
Obesity
Gastroesophageal reflux (GERD) also known as indigestion
Allergies
Cancer
Hypertension
All the health conditions listed are related to lifestyle behavior choices. All are preventable or reversible with a well designed workplace wellness program. Unfortunately, most current workplace wellness programs are not specifically designed to prevent or reverse these conditions. There are exceptions, but “workplace wellness” usually means a fitness program, a weight management program, a disease screening program, and advice to take prescribed medications. The standard “healthy” diets recommended by weight management programs often make health problems such as depression, chronic pain and GERD worse.
The Rand Report on Workplace Wellness sponsored by the U.S. Departments of Labor
and Health and Human Services and released in May 2013 found that the
 average participant in workplace wellness
average participant in workplace wellness
programs did not have significant weight loss. After 3 years of participation the average 5’4″ woman weighing 165 pounds lost an average of 0.9 pounds a year and the average 5’9″ 195 pound man lost 1 pound. Seriously! 3 pounds lost after 3 years of effort!?!
In April 2013 the California State Legislature commissioned a study to determine the effectiveness of wellness programs. Researchers at the University of California analysed dozens of existing studies of workplace wellness programs and found that participating in work-based wellness programs did not lower blood pressure, blood sugar or cholesterol and rarely led to weight loss.
It is not surprising then that less than half of employees participate in the wellness programs offered by their employers. Only 46% of employees get a wellness physical exam or complete a health risk assessment (HRA). Far fewer participate in fitness (21%), smoking cessation (7%), weight loss (10%) or disease management programs (16%). Participation rates are expected to increase in 2014 when the Patient Protection and Affordable Care Act (Obamacare) allows employers to shift health care costs to employees and penalize them financially for not participating in wellness programs or achieving desired health outcomes. This is unfair to employees if employers choose to implement “wellness” programs that are not effective. Employers have to chose programs that actually make employees well and produce ROI not only to the employer but to the employees who spend time and effort to participate.
Participation rates are expected to increase in 2014 when the Patient Protection and Affordable Care Act (Obamacare) allows employers to shift health care costs to employees and penalize them financially for not participating in wellness programs or achieving desired health outcomes. This is unfair to employees if employers choose to implement “wellness” programs that are not effective. Employers have to chose programs that actually make employees well and produce ROI not only to the employer but to the employees who spend time and effort to participate.
Employers surveyed for the Rand Report were unaware of the ineffectiveness of their workplace wellness programs. They “overwhelmingly expressed confidence that wellness programs” would reduce costs. Only about half had actually evaluated program impacts and only 2% reported actual savings estimates. Only one company had requested an assessment of cost trends from it’s health plan. Analysis of cost data suggested that participation in a wellness program over 5 years was associated with lower health care costs and decreased health care use which resulted in a total average annual cost saving of $157, this was not statistically significant. This analysis did not take absenteeism and presenteeism cost savings into account, but even so, if the average employer spends $521.00 per employee on vendor costs and program incentives, no math is needed to see that there is no ROI.
per employee on vendor costs and program incentives, no math is needed to see that there is no ROI.
The myth of ROI from wellness programs stems partly from a January 2010 Health Affairs article “Workplace Wellness Programs Can Generate Savings,” Professor Katherine Baicker estimated that medical costs would fall about $3.27, and absent day costs would fall by $2.73 for every dollar spent on wellness programs. Those figures have been widely quoted by wellness vendors in their sales promotion materials but there has been no evidence from actual wellness programs to support these figures. On NPR Marketplace Professor Baicker, admitted that it was “it’s too early to tell.” Johnson & Johnson, the most renowned state-of-the art award-winning workplace wellness program will not disclose it’s ROI numbers or the overall cost of its wellness program. Safeway the company that inspired the incentives/penalties in Obamacare has actually seen increased cost trends since their wellness program started in 2009 and have not released recent ROI reports.
One of the reasons for lack of significant health improvements from wellness programs is the focus on exercise.  Exercise is an easy target. The design of most wellness programs is based on the myth that people are overweight and have health problems because they are lazy and don’t get enough exercise. If you do a random survey of the overweight people you know, you may be surprised to find that most are walking or going to a gym or work in a job with high physical demands. The problem is not lack of exercise but that exercise alone does NOT produce weight loss. The average person quits after about 8 weeks of no results on an exercise program. Those who stay with the program may be fitter and believe they are healthier but exercise does NOT unclog arteries. if arteries are clogged the employee is at risk of having a costly heart attack or stroke. In fact they are more likely to have a heart attack while exercising.
Exercise is an easy target. The design of most wellness programs is based on the myth that people are overweight and have health problems because they are lazy and don’t get enough exercise. If you do a random survey of the overweight people you know, you may be surprised to find that most are walking or going to a gym or work in a job with high physical demands. The problem is not lack of exercise but that exercise alone does NOT produce weight loss. The average person quits after about 8 weeks of no results on an exercise program. Those who stay with the program may be fitter and believe they are healthier but exercise does NOT unclog arteries. if arteries are clogged the employee is at risk of having a costly heart attack or stroke. In fact they are more likely to have a heart attack while exercising.
Another reason for no ROI is the belief that screening for disease is wellness. Screening based on the US Preventive Service Task Force guidelines is recommended but unnecessary screening increases costs. If the outcome of screening is medication management instead of lifestyle changes employees may actually be less productive.  Cholesterol lowering statin drugs are good example, the FDA warns that statins may increase the risk of diabetes, memory loss, mental confusion, forgetfulness, muscle damage and liver injury. Most physicians firmly believe that the benefits of these drugs outweigh the risks but a 2008 study found that over 2/3 of the people hospitalized for heart attacks had cholesterol levels within the normal range. Approximately 21% were currently taking stains. Statins may stabilize atherosclerotic plaques but they DO NOT unclog arteries. The ONLY non-surgical way to unclog arteries is to adopt a plant-based diet. Plant-based diets also reverse diabetes. Unclogging arteries improves mental and physical function by increasing blood flow to the brain and other vital organs. Educating employees about plant-based nutrition is a low-cost approach that produces real wellness and ROI.
Cholesterol lowering statin drugs are good example, the FDA warns that statins may increase the risk of diabetes, memory loss, mental confusion, forgetfulness, muscle damage and liver injury. Most physicians firmly believe that the benefits of these drugs outweigh the risks but a 2008 study found that over 2/3 of the people hospitalized for heart attacks had cholesterol levels within the normal range. Approximately 21% were currently taking stains. Statins may stabilize atherosclerotic plaques but they DO NOT unclog arteries. The ONLY non-surgical way to unclog arteries is to adopt a plant-based diet. Plant-based diets also reverse diabetes. Unclogging arteries improves mental and physical function by increasing blood flow to the brain and other vital organs. Educating employees about plant-based nutrition is a low-cost approach that produces real wellness and ROI.
 Choices have consequences, asking employees to take responsibility for their health and pay for their poor health choices is not a bad idea, but they may also be paying for the poor choices of their employers. If an employer chooses an ineffective wellness program that results in more medications and no real health improvement, then it is unfair to penalize employees for not participating or not achieving expected health outcomes. Employers who plan to penalize employees for their health choices should be sure that their wellness program is worth the effort of participation.
Choices have consequences, asking employees to take responsibility for their health and pay for their poor health choices is not a bad idea, but they may also be paying for the poor choices of their employers. If an employer chooses an ineffective wellness program that results in more medications and no real health improvement, then it is unfair to penalize employees for not participating or not achieving expected health outcomes. Employers who plan to penalize employees for their health choices should be sure that their wellness program is worth the effort of participation.
 There are effective workplace wellness programs: the program at GEICO is an example. In 2010 the Physicians Committee for Responsible Medicine (PCRM) conducted a study at GEICO headquarters that focused on changing the eating habits of employees. The average participant in this study lost 11 pounds in 22 weeks. A more recent geographically diverse study of GEICO workers in 10-cities produced an average weight loss of 6.4 pounds in 18 weeks.
There are effective workplace wellness programs: the program at GEICO is an example. In 2010 the Physicians Committee for Responsible Medicine (PCRM) conducted a study at GEICO headquarters that focused on changing the eating habits of employees. The average participant in this study lost 11 pounds in 22 weeks. A more recent geographically diverse study of GEICO workers in 10-cities produced an average weight loss of 6.4 pounds in 18 weeks. At an average of 0.4 pounds per week the 195 pound man in the Rand study who only lost a pound a year would have lost 20 pound a year and be in the normal BMI range in the second year of the program, without increasing physical activity. Some workers such as manufacturing and production workers may get the recommended amount of physical activity at work. Office workers would be encouraged to start an exercise program to maintain weight loss. An exercise program is ideal for weight and heath maintenance but NOT for weight loss or disease reversal
At an average of 0.4 pounds per week the 195 pound man in the Rand study who only lost a pound a year would have lost 20 pound a year and be in the normal BMI range in the second year of the program, without increasing physical activity. Some workers such as manufacturing and production workers may get the recommended amount of physical activity at work. Office workers would be encouraged to start an exercise program to maintain weight loss. An exercise program is ideal for weight and heath maintenance but NOT for weight loss or disease reversal
 The most effective wellness programs include evidence-based nutrition, stress management, relationship skills and fitness assessments with activity prescriptions. The intervention should be followed by monthly follow-up sessions to help employees to sustain healthy habits. The program should interface with primary care physicians because participating employees are usually able to stop or require less medications for diabetes, blood pressure and heart disease.
The most effective wellness programs include evidence-based nutrition, stress management, relationship skills and fitness assessments with activity prescriptions. The intervention should be followed by monthly follow-up sessions to help employees to sustain healthy habits. The program should interface with primary care physicians because participating employees are usually able to stop or require less medications for diabetes, blood pressure and heart disease.
References
Loeppke, R, et. al. Health and Productivity as a Business Strategy: A Multi-employer Study JOEM 51(4):411-428, April 2009 http://www.ncbi.nlm.nih.gov/pubmed/19339899
Mishra, S, et. al. A multicenter randomized controlled trial of a plant-based nutrition program to reduce body weight and cardiovascular risk in the corporate setting: the GEICO study, European Journal of Clinical Nutrition (2013) 67, 718–724; doi:10.1038/ejcn.2013.92; published online 22 May 2013 http://www.nature.com/ejcn/journal/v67/n7/full/ejcn201392a.html
Ferdowsian HR, Barnard ND, Hoover VJ, Katcher HI, Levin SM, Green AA et al. A multicomponent intervention reduces body weight and cardiovascular risk at a GEICO corporate site. Am J Health Promot 24: 384–387.
Sachdeva, A, et al. Lipid levels in patients hospitalized with coronary artery disease: An analysis of 136,905 hospitalizations in Get with the Guidelines, American Heart Journal – January 2009, 157 (1) 111-117.
Consumer Updates: FDA Expands Advice on Statin Risks, Apr 12, 2013, DHHS, FDAwww.fda.gov/ForConsumers/ConsumerUpdates/ucm293330.htm
B-12 Supplement
Heart Attack Risk Calculator
BMI Calculator
ALM on Facebook
Error :
- A feed could not be found at `http://www.facebook.com/feeds/page.php?id=1416121451938478&format=rss20`; the status code is `404` and content-type is `text/html; charset="utf-8"`
RSS Feed currently unavailable.

